By: Deaysha Hines, DO
Editor’s Note: Dr. Deaysha Hines was a medical student on the FACTS elective when she summarized this thorough editorial article [1] published in Ultrasound in Obstetrics & Gynecology in 2011. Stuart Campbell penned the editorial as a call to action in response to an article by Hassan et al [3] addressing a specific approach to reduce the rising incidence of spontaneous preterm birth. Campbell’s review of the topic, including findings from Hassan et al and others, led to the conclusion that universal cervical-length ultrasound screening at mid-term followed by daily vaginal progesterone in women identified as high risk would lower the incidence of early spontaneous preterm birth in a cost-effective way free of side effects.*
Introduction
Progesterone supplementation can be used to establish a better luteal phase to support implantation and sustain pregnancy. The editorial article by Campbell [1] summarized below explores the use of vaginal progesterone on women with short cervical length to reduce the number of preterm births and associated neonatal morbidity and mortality. Campbell’s article also provided evidence of the cost-effectiveness of implementing this proposed screening and prophylactic treatment.
“Progesterone supplementation can be used to establish a better luteal phase to support implantation and sustain pregnancy.”
The article was published in 2011 and showed that over the previous forty years, despite advances in technology and medicine, the rate of preterm birth remained virtually unchanged at 12.5% in the U.S. and 5-9% in other developed countries. In some of these countries, preterm births increased in that span of time, with some attributed to assisted reproductive technology. At that time, spontaneous preterm birth had the highest impact on morbidity and mortality in deliveries less than 32 gestational weeks, accounting for 1-2% of all preterm deliveries and 60% of perinatal mortality.
Data Review on Progesterone Supplementation
Campbell’s article [1] summarized studies to date on progesterone supplementation. The evidence showed progesterone did more than block uterine myometrial contraction before the time of delivery. It also maintains pregnancy through mediation of proinflammatory cytokines and decreased antibody production. Although spontaneous uterine activity does occur following progesterone withdrawal, this is not the earliest indicator of preterm delivery. As observed via transvaginal ultrasound, cervical length and ripening occur weeks before uterine contractions and are better signs to assess in screening and potentially preventing preterm birth.
“The evidence showed progesterone did more than block uterine myometrial contraction before the time of delivery. It also maintains pregnancy through mediation of proinflammatory cytokines and decreased antibody production.”
Elevated amniotic fluid cytokine levels have a 22% increased incidence within cervical lengths less than 15mm, increasing the risk of preterm birth. In terms of luteal support in implantation and early pregnancy rates, studies of progesterone supplementation showed vaginal micronized progesterone as the best form compared to natural progesterone (oral or intramuscular) or synthetic progestins. It had very few side effects and can also be used to prevent spontaneous preterm births. Progesterone dosing for prophylaxis of spontaneous preterm birth was shown to be one-third the amount needed for luteal support, around 90-100 mg vaginal progesterone bioadhesive gel.

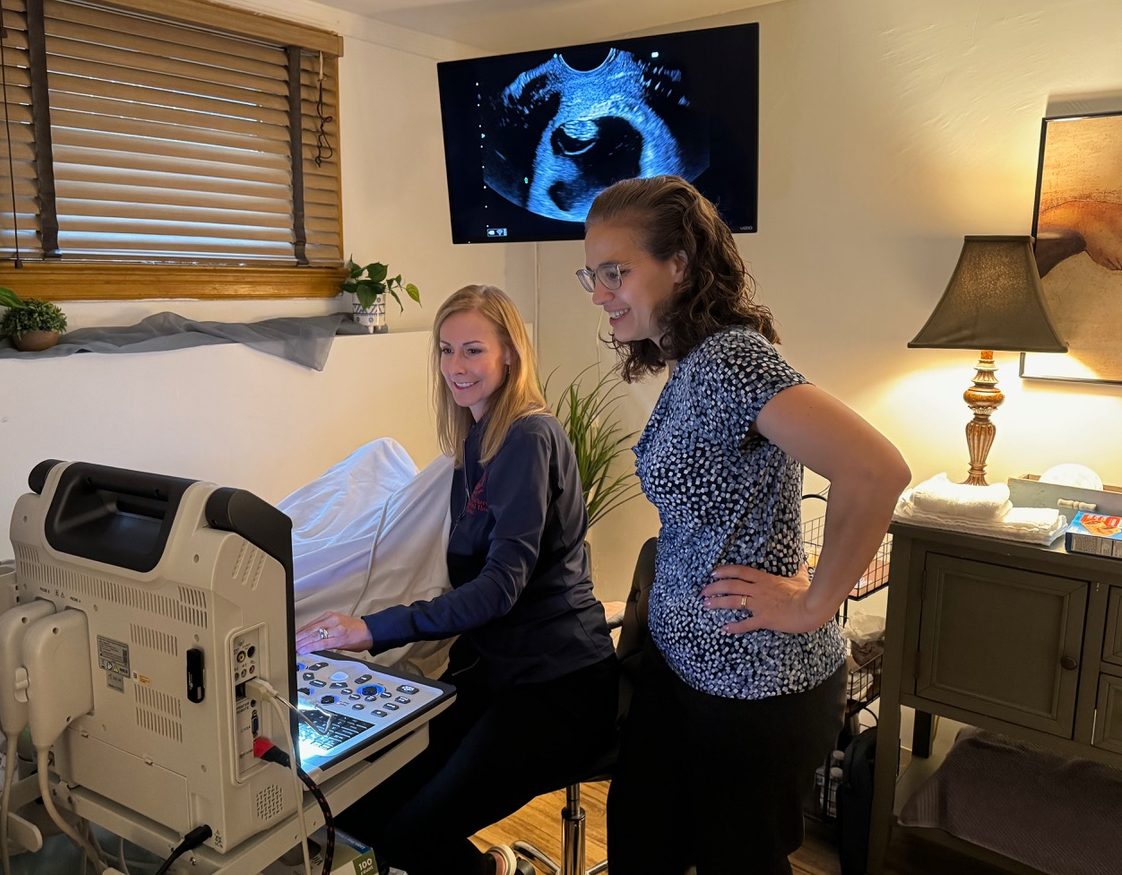
Data Review on Cervical Length Screening
Two multicenter trials studied transvaginal ultrasounds for cervical length screening in the second trimester. Fonseca et al [2] performed transvaginal ultrasounds during gestational weeks 22 to 25, treating women with cervical lengths <15mm. This protocol resulted in 40% less spontaneous preterm deliveries before 34 weeks compared to the placebo control group. Hassan et al [3] conducted transvaginal ultrasounds during gestational weeks 19 to 24, treating women with cervical lengths between 10 and 20mm. Their study also resulted in a significant reduction; specifically, they saw 45% less spontaneous preterm births before 33 weeks compared to the placebo control group, a 50% reduction in preterm birth before 28 weeks, and significant reductions in infants with very low birth weights and respiratory distress syndrome, two common complications of preterm birth.
Their study also reviewed the potential role of vaginal progesterone in reducing preterm births with twin gestations and the optimal cervical length range. A cervical length <10mm showed no effect on preterm birth rate with vaginal progesterone supplementation at a dose of 90-100mg. They also studied the inclusion of cerclage as another possible intervention, which has shown to only help in women with a history of preterm birth <35 weeks gestation and current singleton pregnancy with short cervical length on transvaginal ultrasound <24 weeks.
Cost Considerations
Campbell’s review concluded that cervical-length screening coupled with progesterone treatment for patients identified as high risk for spontaneous preterm birth is cost effective. [1] Preterm birth prophylaxis reduces the overall cost of perinatal care for babies born preterm as well as estimated care within the first year of life, which can exceed $5.6 billion in the U.S. By reducing spontaneous preterm births, the associated cost can be reduced or eliminated for patients and their families. Further research could also assess the reduction in costs associated with low birth rates and respiratory distress syndrome, which were noted to be less prevalent in the vaginal progesterone supplementation group as compared to placebo.
“Campbell’s review concluded that cervical-length screening coupled with progesterone treatment for patients identified as high risk for spontaneous preterm birth is cost effective.”
Discussion
Campbell’s article [1] and the various studies he cited highlight the role of supplemental progesterone in early pregnancy maintenance and prevention of preterm birth. The research into the use of vaginal progesterone supplementation to prevent preterm birth uses principles and techniques common to restorative reproductive medicine (RRM), such as vaginal progesterone supplementation during the luteal phase to support implantation and maintenance of pregnancy. RRM protocols have used vaginal progesterone supplementation for luteal support in dosages three times the amount needed for preterm birth prophylaxis with limited side effects.
Progesterone helps keep the uterus free from proinflammatory cytokines and prevents preterm birth by strengthening the cervix. In the absence of progesterone, the release of proinflammatory cytokines results in cervical softening and effacement. The best way to choose which women to treat with progesterone prophylaxis is with transvaginal ultrasound screening to measure cervical length during gestational weeks 19 and 24 of single gestation pregnancies. Women with uterine cervical length of 10 to 20 mm are at higher risk of preterm birth and may benefit more from prophylactic vaginal progesterone.
“The best way to choose which women to treat with progesterone prophylaxis is with transvaginal ultrasound screening to measure cervical length during gestational weeks 19 and 24 of single gestation pregnancies.”
The impact of decreasing preterm births less than 32 weeks gestation may seem small, since it accounts for 1-2% of preterm births. However, decreasing the associated perinatal mortality and related consequences and costs can have significant implications for patients and their families, and it is worth ongoing study.
*Editor’s Note: In 2023, ACOG’s “Updated Clinical Guidance for the Use of Progestogen Supplementation for the Prevention of Recurrent Preterm Birth” recommended considering vaginal progesterone as a treatment option for patients with: (1) prior history of preterm birth, (2) singleton gestation, and (3) a shortened cervix identified via ultrasound during the second trimester. Readers are encouraged to read the newer studies (including a meta-analysis) and recommendations on this important topic.
References
[1] Campbell, S. (2011), Universal cervical-length screening and vaginal progesterone prevents early preterm births, reduces neonatal morbidity and is cost-saving: doing nothing is no longer an option. Ultrasound Obstet Gynecol, 38: 1-9. https://doi.org/10.1002/uog.9073
[2] Fonseca EB, Celik E, Parra M, Singh M, Nicolaides K. Progesterone and the risk of preterm birth among women with a short cervix. New Engl J Med 2007; 357: 462–469.
[3] Hassan SS, Romero R, Vidyadhari D, Fusey S, Baxter JK, Khandelwal M, Vijayaraghavan J, Trivedi Y, Soma-Pillay P, Sambarey P, Dayal A, Potapov V, O’Brien J, Astakhov V, Yuzko O, Kinzler W, Dattel B, Sehdev H, Mazheika L, Manchulenko D, Gervasi MT, Sullivan L, Conde-Agudelo A, Phillips JA, Creasy GW for the PREGNANT Trial. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 2011; 38: 18–31.
ABOUT THE AUTHOR
 Deaysha Hines, DO
Deaysha Hines, DO
Deaysha Hines, DO is a first-year resident in internal medicine at Nazareth Hospital. She earned her medical degree at Philadelphia College of Osteopathic Medicine in Philadelphia, PA and completed her undergraduate education at Villanova University in Villanova, PA. Dr. Hines is interested in health education and bridging social determinants of health. She enrolled in the FACTS elective to learn more about fertility awareness-based methods to expand her knowledge of women’s health and provide a broad array of options to patients for their reproductive and overall health.
Inspired by what you read?
You can support the ongoing work of FACTS here. To connect with a member of our team, please email development@FACTSaboutFertility.org. Interested in becoming an individual or organizational member? You can learn more and register here. To discuss with a member of our team, please email members@FACTSaboutFertility.org.