Learn with FACTS
External signs or biomarkers provide an overview of reproductive functioning. Observing and recording this information routinely allows women to be active participants in monitoring their health.
Irregularities such as a change in cycle length, painful periods, abnormal bleeding, inability to conceive, or other gynecologic concerns such as polycystic ovarian syndrome (PCOS) and endometriosis, may reflect underlying hormonal abnormalities.
Charting this information each day can provide key information to help trained clinicians diagnose health problems and treat various conditions over the course of women’s reproductive life.
Healthy men are almost always fertile, while healthy women are almost always infertile. FABMs promote a couple’s shared responsibility, communication, and intimacy.
Daily observations of physical signs or biomarkers that change throughout a woman’s menstrual cycle indicate when a woman may be fertile.
Using this information, couples may time sexual intercourse according to their desire to achieve or avoid a pregnancy.

Cervical fluid secretions can be noted throughout the day, either through sensation and/or visual observations. Variations in cervical mucus reflect hormonal changes that affect the cervix.

An increase in the resting body temperature is an indicator of rising progesterone that can be detected after ovulation.

Byproducts of the hormones present can be measured in the urine stream, just as one would take a pregnancy test.

Short, regular, or long cycles can be defined by knowing your total cycle length.
Through learning a natural or fertility awareness-based method.
Fertility awareness-based methods (FABMs) are methods in which a woman observes external signs that reflect underlying hormonal changes, notes them in a chart, and combines that information with an effective set of instructions to help identify the times of a woman’s cycle when pregnancy can and cannot occur. These methods are cost effective and easy to use.
Fertility awareness-based methods differ significantly from conventional forms of birth control, as FABMs are natural, have no medical side effects, and allow a woman to cooperate with her body without suppressing her normal physiology.
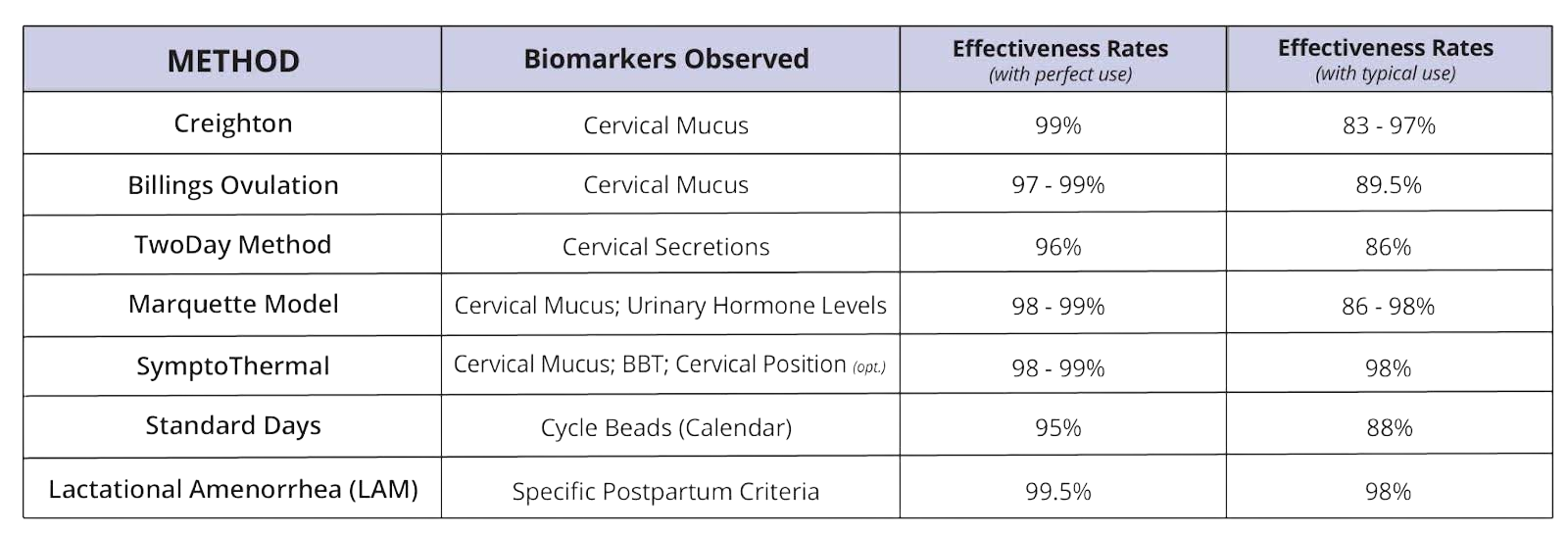
There are different types of modern, evidence-based FABMs that support family planning and health monitoring. Based on the highest quality research studies, typical use effectiveness rates for FABMs range from 86% – 98% for pregnancy prevention.
It is important to note that the effectiveness rates of an FABM depends on the person’s willingness to learn the method from a qualified teacher, motivation to use it correctly, and cooperation or support from her male partner.
Some FABMs work no matter the cycling pattern of an individual woman. For example, the Billings Ovulation Method® (BOM), Creighton Model, SymptoPro, CCL Sympto-Thermal and sympto-hormonal methods and the Marquette model can all be used by women with long or short cycles when discontinuing hormonal contraception, as well as during breastfeeding and during perimenopause. The Standard Days method and the original Calendar Rhythm method however, require regular menstrual cycles because they are based upon a woman’s cycle history.
It should be noted that most modern methods provide information in “real time.” They are based upon a woman’s day-to-day observations where she can make decisions about her fertility based upon those observations.
Trained FABM instructors can provide women or couples with specific guidelines to learn how to best apply the method to their individual circumstances. It may not necessarily mean extended periods of sexual abstinence, but it may require additional instruction when help is needed.
Yes. Charting can help a woman to see how stress is affecting her cycle and her fertility. For example, if a woman experiences a stressful event or illness in the preovulatory phase, ovulation will typically be delayed, leading to a longer cycle.
If a stressful event or illness occurs in the postovulatory phase, this phase may become shorter than normal, and menses will happen earlier than expected. Generally, the luteal phase is a set number of days for each woman (between 12-16 days), and longer cycles reflect long follicular phases, which may be due to stress, illness, or a number of other factors. Daily observations through charting can help a woman to monitor these effects.
A large trial of the Billings Ovulation Method® (BOM) in India by the Indian Council of Medical Research Task Force on NFP (1996) followed 2059 women, the majority of whom were illiterate. In this patient population, the perfect use rate was 1.1 pregnancies per 100 woman-years, with a typical use unintended pregnancy rate of less than 2% pregnancies per 100 woman-years.
The World Health Organization conducted a multi-continent study including many uneducated women and found that 94% of the women taught NFP were able to identify their fertile symptoms correctly on the first cycle.
Despite the challenge of avoiding intercourse during fertile times, surveys of persons using these methods often show that couples have more satisfying sex lives, improved relationships, and feel more respected by their partners and in control of their fertility.
A key factor relates to a couples’ level of emotional maturity and also whether they mutually agree on common goals to achieve or avoid pregnancy. Each FABM addresses this concern. Many FABMs provide relationship building techniques for couples to use during the fertile time if they are abstaining. Further, every successful relationship requires some self-control and sacrifice, and many couples find that this brief time of discipline helps to strengthen their relationship.
The overwhelming majority of FABM effectiveness studies involve couples avoiding genital contact during the fertile phase, with a few exceptions. Condoms or barriers are other forms of contraception that some couples choose to use in addition to using an FABM. However, condoms have an effectiveness rate of their own that is lower than evidence-based FABMs. Couples who choose to combine methods should expect an effectiveness rate of the less effective method they use.
Women may use the Lactational Amenorrhea Method (LAM) if they are within 6 months of delivery, have not had a return of menses, and are near exclusively breastfeeding. If they meet all three criteria, they will have an unintended pregnancy rate of less than 2%.
When a woman no longer meets the above criteria and has not had a return of regular cycles, then most FABMs will advise relying on the mucus pattern (including observations and sensation). The presence of cervical fluid will give an indication of the return to fertility. “Patches” of mucus may appear before the actual build up to ovulation. Any change from a dry mucus pattern should be presumed “possibly fertile.” Additionally, some women experience a constant mucus pattern during this time. A certified instructor can help the woman to determine what her “unchanging pattern” is and to treat that as if it were her own “dry” pattern. She would then be instructed to consider any change from that as possibly fertile
The Billings Ovulation Method® (BOM), Creighton Model, SymptoPro and CCL Sympto-Thermal methods and the Marquette model all provide specific guidelines for women with special situations, such as women who are breastfeeding or are premenopausal. It is important for women and couples to work with their trained instructors to ensure they are using their respective method correctly given their reproductive situations.
Specific postpartum instructions will vary by FABM, and patients should work with their instructor for guidance with monitoring their return to fertility.
Stay connected with timely news, blog postings, and upcoming events with FACTS.